Ono Pharmaceutical considers open innovation as a lifeline, and is collaborating with leading-edge biotechnology companies and academia in Japan and overseas in efforts to produce innovative new treatments. In addition to conventional small-molecule drugs and antibody drugs, we are proactively engaged in modalities (drug discovery platform technologies) including RNA-targeted medicines and cell therapy, with the aim of offering patients new treatment options.
Small molecule, mid-size molecule, nucleic acid
Biologics
Case Examples
Bispecific Antibody
In April 2014 and March 2018, Ono entered into a drug discovery collaboration with Merus N.V. (Utrecht, the Netherlands; hereinafter, “Merus”) aimed at the development of new drug candidates in the field of autoimmune diseases. During this collaboration, we worked together to develop bispecific antibodies using Merus’ proprietary Biclonics® technology, whereby we created ONO-4685 and ONO-4915.
- ONO-4685 is a bispecific antibody that recognizes the two molecules PD-1 and CD3 as antigens. ONO-4685 offers hope in eliminating and attenuating activated T cells, therefore phase I clinical trials are currently underway for autoimmune diseases. In addition, because it induces cytolytic activity in PD-1 expressing lymphoma cells, phase I clinical trials are currently underway for T-cell lymphomas.
- ONO-4915 is a bispecific antibody that recognizes the two molecules PD-1 and CD19 as antigens. ONO-4915 offers hope in attenuating activated B cells and activated T cells, therefore phase I clinical trials are currently underway for autoimmune diseases.
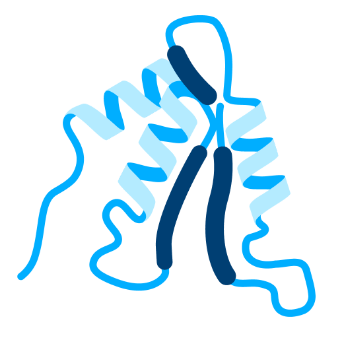
What Are Bispecific Antibodies?
Antibodies that occur in the natural world can usually only bind with one antigen, but a bispecific antibody has been artificially modified using, for example, genetic recombination technology, so that the one antibody is able to simultaneously bind with two different antigens or with two different sites on the same antigen. Through this, it is hoped that it produces effects that were difficult with conventional antibody drugs, such as inhibiting the function of two antigens simultaneously, or conveying specific cells to a targeted location, and research and development is therefore underway to produce therapeutic agents for various disorders, particularly cancer.
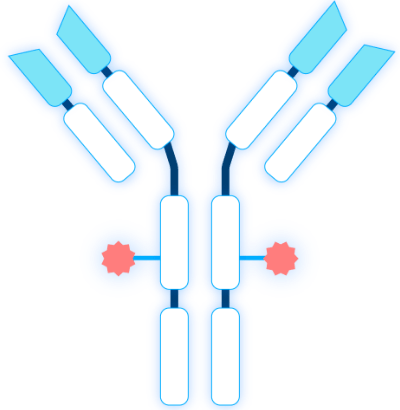
Antibody-Drug Conjugate (ADC)
In October 2024, Ono entered into a license agreement with LigaChem Biosciences, Inc. (Daejeon, South Korea; hereinafter, “LCB”) for LCB97, a new drug candidate in the field of solid tumors, and a drug discovery collaboration using LCB’s proprietary antibody-drug conjugate (ADC) technology, ConjuAll™ platform to develop novel ADCs. LCB97 is a first-in-class ADC developed to target L1 cell adhesion molecule (L1CAM) which has been reported to be highly expressed in multiple solid tumors, with the aim of delivering a new means of treatment for cancer patients for whom treatment had previously been difficult. In addition, this drug discovery collaboration for developing novel ADCs using the ConjuAll™ platform aims to develop new ADCs to target cancer antigens other than L1CAM.
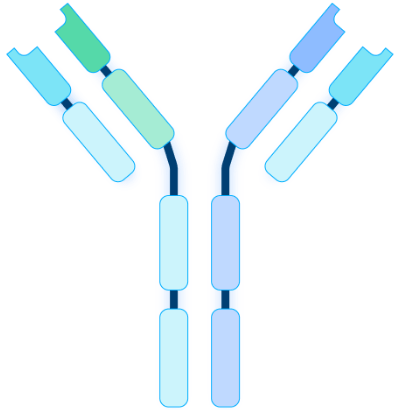
What Are Antibody-Drug Conjugates (ADCs)?
Antibody-drug conjugates (ADCs) are a type of biopharmaceutical that combines an antibody that targets specific cells with a highly potent active pharmaceutical compound. They are recently attracting much attention as a form of cancer treatment. By delivering chemotherapy agents directly to cancer cells, it reduces the impact on health cells compared with conventional chemotherapy, and can be expected to reduce side effects.
Cell Therapy
In September 2018, Ono entered into a drug discovery collaboration with Fate Therapeutics (CA, USA; hereinafter “Fate”) for the development of iPS cell-derived chimeric antigen receptor (CAR)-T cell therapeutic agents. This partnership aims to overcome the major problems faced by conventional CAR-T cell therapy in the treatment of solid tumors, such as the heterogeneity of tumor antigens, immunosuppression in the tumor microenvironment, and the low infiltration of CAR-T cells to tumors, with the aim of delivering a new means of treatment for cancer patients for whom treatment had previously been difficult.
In this partnership, Ono combined the new cancer-selective anti-HER2 antibody H2CasMab-2 obtained by Yukinari Kato, M.D., Ph.D. (Department of Antibody Drug Development, Tohoku University Graduate School of Medicine) with Fate's cutting-edge iPSC product platform, in order to develop the iPSC-derived HER2 CAR-T cell therapy ON0-8250/FT825. The anti-HER2 antibody H2CasMab-2 was originally generated by Dr. Kato as a result of the Science and Technology Platform Program for Advanced Biological Medicine of the Japan agency for Medical Research and Development (AMED). Ono is working in conjunction with Fate in the U.S. and Europe, while having an exclusive license to develop and commercialize the cell therapy in other regions, and is currently conducting phase I clinical trials in the U.S.
What Is iPSC-Derived CAR-T Cell Therapy?
It is a treatment administered to patients that uses induced pluripotent stem cells (iPSC) to produce large volumes of CAR-T cells that detect and attack cancer cells. Because conventional CAR-T cell therapy uses the patient’s own T-cells, it was necessary to individually harvest and process cells, but with Fate’s platform, it is possible to mass-produce off-the-shelf homogeneous CAR-T cells from genetically edited iPSC. In this way, it offers hope of stable quality and supply, as well significant cost reduction, without the need to harvest cells from individual patients or donors. Also, through multiple gene editing, we aim to improve transferability to tumors and immunosuppression resistance, for effective treatment of solid tumors.
Content reflects information available in December 2025
